Introduction to person centred care
- Categories: Best Practice & Advice, Ebooks
Joe Webber
Share this article
Download your free ebook!
Don’t forget to grab your copy of our free Introduction to Person-Centred Care ebook…
Contents
- Introduction
- What is person-centred care?
- The importance of person-centred care
- What are the benefits of person-centred care?
- Benefits for residents
- Benefits for care providers
- How to achieve person-centred care
- Person-centred care planning
- How can technology support person-centred care?
- Tips for person-centred care
Introduction
‘Person-centred’ is a term that’s become embedded within the UK’s care sector over recent years. Its importance to individual wellbeing is thoroughly documented, and the practice is endorsed by national organisations including the NHS, and regulatory bodies like the Care Quality Commission. A person-centred care service is currently the gold standard of care provision, offering numerous benefits for care residents, staff and business owners.
As the sector steadily moves toward accomplishing the goal of adopting and maintaining a complete person-centred approach to care, older ways of operating are gradually becoming obsolete. Care providers that have embraced personalised care are better equipped to evidence a safe, effective, responsive and caring service. These components are necessary to enable resident fulfilment, staff happiness and the best possible inspection results.
This ebook covers the basics of person-centred care, including the benefits, the role care planning plays, how technology can support and our top tips.
What is person-centred care?
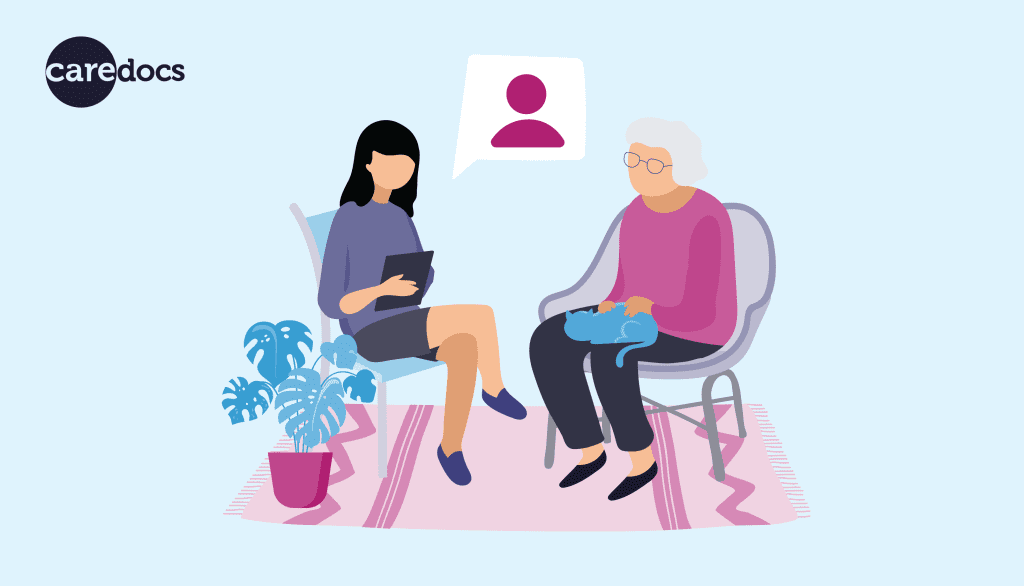
At its foundation, person-centred care (or patient-centred care) is a service which puts the needs of the individual first. When care and treatment is highly personalised, it becomes much more effective, and this is the key to driving better performance across many areas of the business. To achieve a person-centred service, a provider must first carry out an assessment to establish the unique needs and preferences of each resident.
For the best results, good communication is essential at all times. Instead of simply asking questions in a fixed order to complete an assessment, discussion should be encouraged to obtain more in-depth information. A care plan can then be formulated in partnership with the individual. By involving them in this process, you’re ensuring their satisfaction with your service right from the start.
Every care provider should strive to offer person-centred care as opposed to a generic or strict service. Not just because it’s a requirement set by, or is in line with, the values of every national care regulatory body in the UK. It’s also a critical factor in ensuring a respectful and dignified care experience.
The importance of person-centred care
Person-centred care is so important to the wellbeing of care home residents for many reasons. It promotes respect, dignity and independence in the community and ensures that people who need care have their voices heard by providing a platform to express themselves. Everybody is given the same chance to succeed and live a fulfilled life, and the job in return becomes more rewarding. Offering a person-centred service builds communication, trust and relationships between residents and care workers.
A resident’s contribution to the care planning process and decision-making in general, is crucial for an efficient service. Without their input it’s not possible to plan or provide tailor-made care or treatment. Person-centred care plans can be time consuming to produce, but time and patience are necessary for effective results. The time spent ensuring your service is person-centred can be thought of as an investment. If done correctly, you should see a decrease in reoccurring issues and new emerging problems in a short space of time.
Person-centred care can also take family and friend input into account. Although this won’t always be necessary, if some residents have trouble communicating or have been looked after by somebody else prior to joining the care business, a third party can help explain what has worked well so far and what to avoid. The more people who support the plan, the more likely it will be to succeed.
What are the benefits of person-centred care?
Benefits for residents
Person-centred care providers are able to offer a service based on each person’s individual needs to ensure the best possible care is delivered. This helps the resident feel included, listened to and valued. Their participation reinforces dignity and independence, and encourages relationship building. By asking the right questions, staff can learn about the preferences and strengths of the people in their care and offer unique and effective solutions. As a result, unwanted or ineffective treatments or activities are significantly reduced.
Having the power to make a choice, no matter how small, can be empowering. Involving residents in the decision-making process makes the service naturally more transparent. Greater transparency can translate into stronger relationships and increased trust. Trust is important because when a person feels more comfortable in their environment, they are more inclined to open up about themselves, raise concerns and ask questions. This all contributes to a more effective care plan.
With the purpose of person-centred care to increase efficiency and improve care – residents will recover quicker from acute and longer-term illnesses and feel more satisfied with the service they receive. Homing in and tackling issues as soon as they’re presented leads to fewer diagnosis tests and referrals. Physical, mental and emotional health will all benefit in some way from receiving a personalised service, resulting in better morale and feedback across the business.
Benefits for care providers
A person-centred approach to care encourages adaptability. So instead of following a single method of care or treatment for long periods of time, a service will be evaluated regularly to ensure its working as intended. Keeping a close monitor on each person’s health while always striving for the most effective solutions, not only supports wellbeing, but significantly helps to reduce time, energy, and money wastage.
Every care plan that is created will be different to fit the specific needs of each resident. Finding creative and innovative solutions to problems encourages more critical thinking from care staff. Trying new ways of working to overcome unique challenges increases experience, confidence and supports collaboration among staff. Residents will greatly appreciate the personalised response, as it shows their concerns and conditions were listened to. Seeing first-hand that your ideas and dedication are having a positive impact makes the job a much more rewarding experience.
Solving problems at the earliest opportunity and working together toward goals evidences that a service is responsive, effective, personalised and caring. These are necessary criteria for receiving top marks in an inspection. Being able to show off great ratings and testimonials from residents increases momentum which in turn generates more business and more profit.
How to achieve person-centred care
Taking a person-centred approach to care begins with conducting a thorough care needs assessment for each resident. This means having detailed conversations about all aspects of daily care and following up with relevant questions. This information can then be used to identify risks, goals and then produce a care plan that focuses solely on the requirements and preferences of the individual.
The care plan should be personalised to high standards and in most cases written from their perspective (first-person). If the individual doesn’t have the capacity to make the majority of decisions for themselves, it might be more appropriate to write it in third-person. When the draft is finished, the documentation should be checked over with the resident or their decision-maker to ensure all parties are satisfied, or to highlight where there is room for improvement.
Care staff can then work from this document to deliver the best quality care and treatment. It should contain everything they need to know about the resident to minimise the need for the individual to repeat themselves. If a more efficient method of care is found, this should be discussed with the person who is receiving care and all parties should be in agreement before making changes.
To support the person-centred experience, residents should be provided with as much information as possible relating to the status of their health to assist in making decisions about their care. If necessary, provide them with informative, educational resources suitable for their level of understanding, to help them become more confident with their treatment plan. Although the resident’s satisfaction is the goal, safety and wellbeing are still priorities of the carer.
Care files should be continuously updated to include the likes, dislikes and general preferences each time new information presents itself. This data can be logged in daily care notes, forms, emotion mapping charts and in the care plan. Care staff can take it into account when proposing activities, care and treatment. This demonstrates that you listen and respect their involvement. It’s also important to take the views of family and friends into consideration to help them get onboard with the service and help them remain supportive.
A person-centred care service needs to be able to adapt in real time. Care plans should be evaluated regularly to ensure they are kept up to date and effective, and reviewed completely at least every six months. When it becomes apparent that the service needs improving, for example, if a treatment isn’t getting the desired results, changes should be documented immediately so inefficient practice doesn’t continue. Therefore, care plans will evidence when ineffective care is caught early and how changes were made to support the resident.

Person-centred care planning
Care plans are, at their core, communication tools. In order to make a care plan person-centred and enable the best possible care, there needs to be a heavy focus on collaboration during the creation process. The assessment is an opportunity for residents to get involved and engage in discussions about personal health and share relevant facts or stories from their lives.
The more transparency and trust there is between care staff and the people in their care, the more likely the resident is to open up and provide useful information. To create an effective plan, there needs to be an agreement on goals, risks, concerns, strengths and limitations, as well as acknowledgement of personal beliefs and values. Once this has all been established, it becomes clearer what type of care would be most suitable in multiple scenarios.
A person-centred care plan is also adaptable and requires evaluating regularly to check its effectiveness. If it’s not generating the desired results, the resident should be consulted. The plan will ideally be changed as soon and often as possible until the outcome fits the brief. This demonstrates during an inspection that you are responsive in your approach, while always aiming for effective care.
With care software in place, assessments, plans, daily notes, preferences and more, can be logged and recorded digitally for ease of access. The ability to share data quickly and involve multiple people in the planning, management and delivery of care, means businesses are able to offer a more holistic and personal service. Information can be logged in real time or located quickly. This reduces the need for residents to repeat themselves, receive inconsistent care, or wait around while admin work is completed.
How can technology support person-centred care?
Person-centred care isn’t a new concept but advances in technology have greatly reduced the effort required to support it on a large scale. A digital system makes data handling much easier to manage. And having quick access to information while maintaining a consistent and efficient service is vital for success. By adopting a digital approach to care, real-time information processing can be seamlessly integrated into daily tasks to enable the most effective care.
For example, by logging any care related item into a digital system like CareDocs, that item becomes immediately available for others who have permission to see. The information can be viewed simultaneously from any location with an Internet connection, on different devices, in just a few seconds. This could be beneficial for a carer starting a new shift, a compliance manager performing quality checks, or the business owner when analysing reports. Having access to the most up to date information at speed plays a major role in person-centred care.
Digital systems can be extremely useful, but they don’t offer clinical advice, and implementing one doesn’t automatically ensure your care becomes person-centred. There needs to be a strong human presence across the entire process. Care software is only used to store and manage information, and support staff with providing care. Every user of technology plays an equally important role in upholding the level of quality, so adequate training must be given before rolling out a new technology across a business. If the tech isn’t being used correctly, it won’t be effective.
With care software, time consuming tasks such as carrying out care assessments and creating care plans become much more engaging, and less admin focused. This extra time quickly adds up, which is time that can be spent focusing on caring or building relationships with residents. CareDocs also keeps track of a number of dates and provides reminders to help you stay on top of work, like updating care plans. By giving you the right tools, everyday tasks are made simpler and more efficient.
The more information you enter into the system through assessments, charts, daily notes and forms, the higher number of analytics and valuable insights you will receive back about your residents. This includes their strengths, behaviours, emotions and preferences. Having all your resident data in one system helps you paint a clearer picture of what is working on an individual basis, and where improvements can be made.
Tips for person-centred care
In order to achieve a true person-centred service, every aspect of your business needs to have a focus on the resident. From the way you communicate, make decisions, present information, record and deliver care; each individual’s own best interest should be taken into account. Here’s our top tips for adding a person-centred touch to your service.
- Take time when creating a care plan. Producing a well-crafted care plan can be time consuming, but it’s an investment for your resident and your business. The more you put into it, the more you’ll get out. A person-centred care plan should reveal a clearer path when deciding the best course of action to take. Learning as much as you can about the individuals in your care at the earliest opportunity will help you achieve this. This approach improves efficiency in addition to making the experience more rewarding for both residents and carers.
- Involve your residents in the decision-making process. Discussing care, treatment, goals, ambitions and activities with residents, and making sure they are on board with all outcomes before moving forward is a major part of a person-centred service. You can easily reinforce independence and dignity by giving people the option to make small choices, share their opinion, or check if they have any questions or concerns. Feeling valued and in control is empowering and vital for good mental wellbeing.
- Record as much information as possible. This applies across all care documentation, not just care assessments. By packing your residents’ daily care notes, forms and charts with as much information as possible, you ensure the service is consistent while evidencing your interest in them as a person. No matter who is on shift, the resident can rest assured there’s a high level of communication between the staff and they have everything they need to continue delivering a safe and effective service.
- Improve communication to build trust. Take time out when possible to interact with residents and practice communication skills. You don’t need to say much – you can show interest and empathy using only face and body language, and by active listening. By promoting equality between staff and residents, it creates a stronger sense of community and support. The greater the bond you have with residents, the more trust is established, which is key for obtaining information that can be used when deciding what action should be taken.
- Ensure residents understand their care. Everybody appreciates clear information. But for residents especially, understanding and feeling connected to the support and care you provide can help them gain the confidence to open up about themselves. Confusion or misunderstandings could have serious implications, such as the wrong medication being taken. Ensure the individual feels confident before your meeting comes to an end by checking if they have any questions. If further guidance is needed, consider supplying additional documentation or presenting the information in a new way.
- Welcome feedback. One of the most effective ways to deliver a better service is to ask for feedback – both directly and anonymously – from residents, staff and visitors. It’s a great opportunity to see where your strengths lie and what could use improving. Taking on new ideas, even as a trial, demonstrates that you’re happy to listen and make changes. This lets the people in your care know they are valued and that your service is aimed at them.
To learn more about CareDocs and how we can help support person-centred care at your business, please book a free demo with one of our friendly Business Development Managers, email sales@caredocs.co.uk or call 0330 056 3333 (opt. 2).
If you require assistance with the CareDocs software, we’re standing by to provide support. Email support@caredocs.co.uk or call us on 0330 056 3333 (opt. 1).
Download your free ebook!
Don’t forget to grab your copy of our free Introduction to Person-Centred Care ebook…
Share this article
Author
Joe Webber
Search
Recent articles
- CareDocs Partners with the Professional Record Standards Body (PRSB) to Support Care Standards Fit for the Future of Digital Care January 30, 2024
- CareDocs Joins the Care Software Providers Association (CASPA), an Independent, Not for Profit Association, Representing Software in the Care Industry January 19, 2024
- CareDocs partners with Bristol Waste to tackle digital poverty January 10, 2024
Recent comments
- 1.2. Assess use of care plans in applying person-centered values - CIPD Writers on What is person centred care planning and why is it important?
- Call tracking tips for care home marketers - Chester Times on The importance of effective communication in care
- Why is effective communication important for positive relationships with individuals in care? - Building-Craft on The importance of effective communication in care