What is the ‘MUST’ score and how can it help assess the risk of malnutrition?
- Categories: Best Practice & Advice, Ebooks
Joe Webber
Share this article
Download your free ebook!
Don’t forget to grab your copy of our free MUST Score ebook to take away…
Malnutrition can affect anybody for a multitude of reasons and cause numerous health issues. It simply means having ‘poor nutrition’ and it’s particularly common in society’s most vulnerable, such as the elderly and those with complex needs. In an adult social care setting, having person-centred care plans for all aspects of your service users’ daily care, including nutrition, is essential so you can monitor the health of each individual and ensure they are receiving the most effective service.
Identifying malnutrition
When a diet doesn’t contain enough nutrients, or contains too many, this can cause malnutrition – a serious condition that can lead to a wide range of health problems. Unintentional weight loss or gain, having low or high body weight, feeling fatigued or weak, regularly being unwell and taking long periods of time to recover, and a general lack of interest in eating or drinking are some typical symptoms to look for.
Millions of people in the UK are malnourished, and most commonly it affects individuals who are suffering from long-term health conditions, those who have trouble swallowing food or people who are recovering from serious injuries and burns. Social factors can also play a major role, for example surviving on a low income, having limited mobility or isolated living. Due to a combination of factors from changing lifestyle and medical needs, anybody over the age of 65 years is naturally more at risk of malnutrition.
Treatment of malnutrition mainly involves changing the diet and getting the balance right, but how you achieve this will depend on the severity of the condition. Some may need to consume more calories or protein, but if the underlying cause of the low caloric intake is due to poor mobility or income related, special advice or support will be needed. If the condition is present because a person cannot physically eat, then puréed foods or medical feeding tubes may be required.
Because everybody has different needs, the best way to prevent malnutrition is to carry out a thorough risk assessment for each service user. This is a person-centred approach to caring which will return the greatest benefits to both parties. It ensures the most effective and beneficial service is being provided so time and resources are not wasted. One of the most commonly used risk assessment tools is ‘MUST’.
What is 'MUST'?
‘MUST’ (Malnutrition Universal Screening Tool) is a widely used tool in care settings, including hospitals, care homes and nursing homes, to assess the risk of malnutrition in adults. It was originally developed in 2003 by the Malnutrition Advisory Group – a standing committee of BAPEN, and has been reviewed regularly since.
The following is an excerpt from the official ‘MUST’ guide created by BAPEN, which best sums up their tool:
‘MUST’ is a five-step screening tool to identify adults, who are malnourished, at risk of malnutrition (undernutrition), or obese. It also includes management guidelines which can be used to develop a care plan.
It is for use in hospitals, community and other care settings and can be used by all care workers.
The five steps as described by BAPEN are:
Step 1: Measure height and weight to get a BMI score using chart provided. If unable to obtain height and weight, use the alternative procedures*.
Step 2: Note percentage unplanned weight loss and score using tables provided.
Step 3: Establish acute disease effect and score.
Step 4: Add scores from steps 1, 2 and 3 together to obtain overall risk of malnutrition.
Step 5: Use management guidelines and/or local policy to develop care plan.
*Measuring ulna length is an alternative procedure for estimating height and measuring MUAC (mid-upper arm circumference) is an alternative procedure for estimating a BMI.
For full guidance, including scoring tables, please view the source: https://www.bapen.org.uk/pdfs/must/must_full.pdf
The 'MUST' score
Adding the BMI score, weight loss score and acute disease effect score together will calculate the overall risk of malnutrition. The total scores and their recommended management guidelines are outlined below.
0 – Low risk (Routine clinical care)
- Repeat screening.
– Hospital – weekly
– Care Homes – monthly
– Community – annually for special groups (E.g. those >75 years)
1 – Medium risk (Observe)
- Document dietary intake for 3 days.
- If adequate – little concern and repeat screening.
– Hospital – weekly
– Care Home – at least monthly
– Community – at least every 2-3 months - If inadequate – clinical concern follow local policy, set goals, improve and increase overall nutritional intake, monitor and review care plan regularly.
2 or more – High risk (Treat*)
- Refer to dietitian, Nutritional Support Team or implement local policy.
- Set goals, improve and increase overall nutritional intake.
- Monitor and review care plan.
– Hospital – weekly
– Care Home – monthly
– Community – monthly
*Unless detrimental or no benefit is expected from nutritional support. E.g. imminent death.
Actions for all risk categories:
- Treat underlying condition and provide help and advice on food choices, eating and drinking when necessary.
- Record malnutrition risk category.
- Record need for special diets and follow local policy.
Actions for obesity:
- Record presence of obesity. For those with underlying conditions, these are generally controlled before the treatment of obesity.
For full guidance, including scoring tables, please view the source: https://www.bapen.org.uk/pdfs/must/must_full.pdf

Calculating ‘MUST’ in CareDocs: The three components
With the kind permission of BAPEN, we have digitised the ‘MUST’ tool and integrated it into the Nutrition / Hydration Care Assessment and Care Plan within CareDocs for an efficient digital experience. By doing this, you can naturally calculate a ‘MUST’ score as you progress through the assessment process, provided the three key components are in place.
When using CareDocs, the data required to calculate the ‘MUST’ score is entered into three different areas of the system. After completing the Care Assessment, the system will automatically pull all the information together and provide you with a final score in your Care Plan, saving you from manually cross-checking your data with the ‘MUST’ score cards. The three components (BMI, weight loss or gain and assessment questions) should be up to date and accurate at the time of generating the draft Care Plan.
Adding a BMI
There are two ways to log a service user’s BMI to CareDocs. The first way is to simply add their height to their CareDocs profile page, which only needs to be done once, then add an up to date Weight Chart entry. The BMI will then be calculated automatically by the system. If it isn’t possible to accurately determine the service user’s height or weight, you can manually add their BMI into the system. For ‘MUST’ score purposes, you can refer to the BAPEN Step 1 BMI score chart.
Alternative methods for estimating height and BMI are included near the end of this article. Our Care Assessment will allow you to input this additional information.
Weight entries
In order for CareDocs to calculate the weight loss percentage there must be a minimum of two weight entries recorded for your service user. The first measurement is the most recent entry available and must have been made within the last 30 days. The second weight measurement will be the highest weight entry available within a period of 3 to 6 months before the most recent entry.
The difference between the two weight measurements will provide a weight loss or gain percentage which is used in calculating the ‘MUST’ score where data is available. If you have difficulty adding accurate weight entries due to the capacity of a service user, we have provided additional questions in the Care Assessment to support you with this component.
Acute Disease Effect (Assessment question)
There is a question within the ‘MUST’ section of the Nutrition / Hydration Care Assessment regarding Acute Disease Effect. The answer you provide is a component in calculating the risk score.
Creating the ‘MUST’ score in the CareDocs Care Plan
The ‘MUST’ risk assessment forms just one part of the wider Nutrition / Hydration Care Assessment in CareDocs. To accurately generate a draft Care Plan that contains a ‘MUST’ score, you need to complete the entire Nutrition / Hydration section to ensure all risks and subjective criteria are taken into account.
Following this, the next step is to create the draft Care Plan. This is a simple process where CareDocs automatically generates a document for you using only the information you have provided. This is also the best opportunity to read through the Care Plan to review and personalise it so it’s as person-centred as possible before setting the plan in place. At the draft stage, in addition to the remainder of the Nutrition / Hydration Care Plan, you will see the ‘MUST’ score, what the specific risks are to the service user and the support you can provide. In the event of malnutrition, you will be given a plan of care to follow.
Depending on how often you update your Care Plans, it will eventually be time to revise the ‘MUST’ score to see how the service user’s health is progressing. Ensure the BMI and weight entries are up to date, or if you measure weight using alternative measurements, have the newest weight loss estimate data ready. You can then perform the ‘MUST’ risk assessment along with the rest of the Care Assessment to calculate the newest score.
Alternative measurements for estimating BMI
If you are unable to accurately determine a service user’s BMI, which is a key component in ‘MUST’, there are alternative methods for estimating the figure to support you in calculating a risk score. Recommended alternatives for estimating height and weight are outlined below:
How to measure ulna length to estimate height for BMI
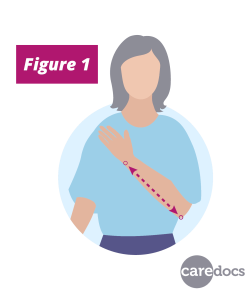
If you already have a weight entry and you require only the height to estimate a BMI, you can estimate a service user’s height by measuring the length of the forearm (ulna). If possible, measure their left side between the point of the elbow and wrist (see Figure 1) and use the BAPEN conversion table below to calculate the estimate.
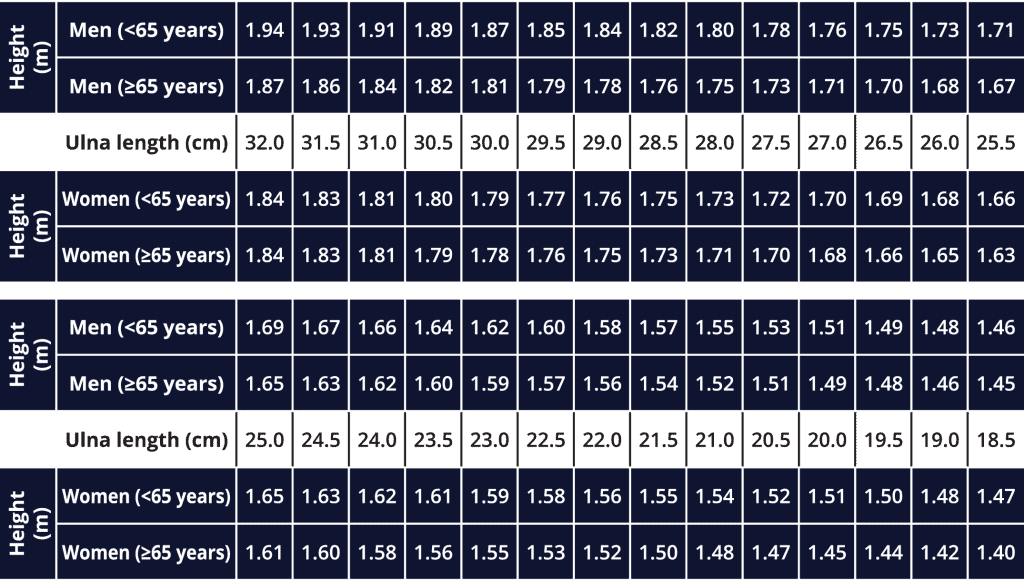
Conversion table originally developed by BAPEN (https://www.bapen.org.uk/pdfs/nsw/nsw11/ulna-measurement-nsw11.doc)
How to measure MUAC to estimate BMI
In the event you cannot accurately measure the height or weight of a service user, measuring the mid-upper arm circumference (MUAC) is an alternative method of loosely estimating BMI and can be performed by following these steps:
Step 1) The service user should be standing or sitting.
Step 2) Use left arm if possible and ensure the arm is bare.
Step 3) Locate the top of the shoulder (acromion) and the point of the elbow (olecranon process).
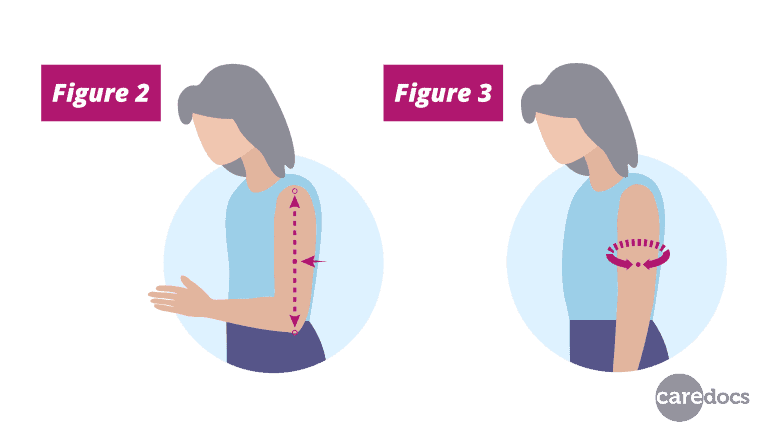
Step 4) Measure the distance between the two points and identify the midpoint and mark on the arm (see Figure 2).
Step 5) Ask the service user to let arm hang loose and with tape measure, measure circumference of arm at the midpoint (Figure 3). Do not pull the tape measure tight – it should just fit comfortably round the arm.
If MUAC is less than 23.5 cm, BMI is likely to be less than 20 kg/m2 (service user is likely to be underweight). If MUAC is more than 32.0 cm, BMI is likely to be more than 30 kg/m2 (service user is likely to be obese). For further information on use of MUAC please refer to the ‘MUST’ Explanatory Booklet.
For more guidance with ‘MUST’, please refer to the BAPEN website. If you require CareDocs support, please contact us at support@caredocs.co.uk.
To learn more about CareDocs either book a free demo with one of our friendly Business Development Managers, email sales@caredocs.co.uk or call 0330 056 3333.
Sources
Malnutrition (NHS): https://www.nhs.uk/conditions/malnutrition/
‘MUST’ (BAPEN): https://www.bapen.org.uk/screening-and-must/must/introducing-must
‘MUST’ full guide (BAPEN): https://www.bapen.org.uk/pdfs/must/must_full.pdf
‘MUST’ calculator (BAPEN): https://www.bapen.org.uk/screening-and-must/must-calculator
Download your free ebook!
Don’t forget to grab your copy of our free MUST Score ebook to take away…
Share this article
Author
Joe Webber
Search
Recent articles
- CareDocs Partners with the Professional Record Standards Body (PRSB) to Support Care Standards Fit for the Future of Digital Care January 30, 2024
- CareDocs Joins the Care Software Providers Association (CASPA), an Independent, Not for Profit Association, Representing Software in the Care Industry January 19, 2024
- CareDocs partners with Bristol Waste to tackle digital poverty January 10, 2024
Recent comments
- 1.2. Assess use of care plans in applying person-centered values - CIPD Writers on What is person centred care planning and why is it important?
- Call tracking tips for care home marketers - Chester Times on The importance of effective communication in care
- Why is effective communication important for positive relationships with individuals in care? - Building-Craft on The importance of effective communication in care









2 Comments
[…] via […]
[…] via […]
Comments are closed.